A power morcellator is a surgical device most commonly used by surgeons to handle a range of surgical procedures. Though used for renal or spleen surgeries, they are also often used by gynecologists to perform myomectomy and hysterectomy procedures. Many surgeons depend on a morcellator during what is known as a robotic surgery, and this is one in which a computer controls the surgical instruments during the actual surgery.
However, a morcellator can also be used manually. The devices allow patients to be operated on laparoscopically, which tends to cut healing time down dramatically. Laparoscopic surgeries for gynecological procedures are an option that many physicians have started to choose over classic “open” surgery or vaginal procedures because they heal faster and are considered more precise.
Laparoscopic procedures use several tools that include cameras, as well as all of the surgical tools necessary, which are run through the tiny tubing that is inserted through the small openings in the patient’s body.
The way the morcellators work is very simple – they use tiny rotating blades that segment large sections of tissue into much smaller ones. When broken into such small pieces, they allow the physician to use the other laparoscopic tools to “vacuum” or suction the pieces out of the body.
Rather than opening a woman’s abdomen and making enormous incisions that take weeks to properly and safely heal, the use of a morcellator allows only a few small incisions (less than 2 cm each). The devices are then inserted into the incisions and the surgical procedure can be done using the tools and the camera mounted into one section of the device.
It is easy to understand why a physician and a patient might appreciate this approach to surgery. After all, the patient does not have larger stomach muscles severed, the amount of pain is dramatically reduced, and the risk of wound complications is almost entirely eliminated. Surgeons use the morcellator because it is minimally invasive and even in light of recent concerns, many gynecologists continue to advocate for the use of the device during hysterectomies and myomectomies.
Have you developed uterine cancer after the use of a power morcellerator?
You may be entitled to compensation.
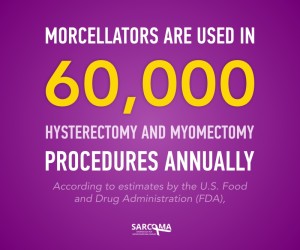
In 2014, the FDA warned against the use of power morcellators during surgical procedures to remove fibroid tumors or during hysterectomies and mymoectomies because of the risk of the spread of cancer. Essentially, the FDA discovered that undetected cancer in the uterus or in fibroid tumors can be easily spread (“seeded”) when the tissue is shredded by the device. Many hospitals and treatment centers have since put moratoriums on the use of power morcellators, even though the rate or instances of cancer have not be completely documented.
Many doctors are going on the record to argue against this move by the FDA, even in light of the fact that the FDA puts the risk of undetected sarcoma from one in three hundred to one in one thousand. In other words, rather than using the more invasive (and cleaner) surgical removal process, the physicians advocate for the use of the morcellator even with such high risk.
Did your fibroid removal give you cancer?
Contact us now.
 It is important to note that sarcomas and Leiomyosarcoma (LMS) in particular, take a lengthy diagnostic process to identify. LMS is not spread via the lymphatic system like other cancers, and actually works its way through the blood stream. The release of diseased tissue and cells, and the risk of leaving even small segments of it behind when using morcellators, puts a patient a great risk for developing a remarkably aggressive form of cancer.
It is important to note that sarcomas and Leiomyosarcoma (LMS) in particular, take a lengthy diagnostic process to identify. LMS is not spread via the lymphatic system like other cancers, and actually works its way through the blood stream. The release of diseased tissue and cells, and the risk of leaving even small segments of it behind when using morcellators, puts a patient a great risk for developing a remarkably aggressive form of cancer.
If you are going to have a hysterectomy or myomectomy, speak with your physician about a procedure that does not involve the use of the morcellator, as it has a proven record of causing patients’ cancer to spread rapidly.
Source
Levitz, Jennifer. Gynecologists Resist FDA Over Popular Surgical Tool. WSJ.com. 2015. http://www.wsj.com/articles/gynecologists-push-back-on-fdas-caution-about-cancer-when-using-morcellation-in-hysterectomies-1411358341