Hysterectomy Cancer
There are many reasons that a woman might be told that a hysterectomy is a good idea, and one of the more common is when she has what are known as “fibroids”. These are benign tumors that almost all women develop during their lives, and yet they can become so difficult and severe as to warrant removal of the tissue (known as a myomectomy) or the entire uterus (known as a hysterectomy).
Leiomyosarcoma Hysterectomy Cancer Risk
 There are different types of hysterectomies, from complete to partial, and most of them are done using specific surgical procedures. For instance, there are “open” hysterectomies in which the patient is opened at the abdomen and the tissue and organs are surgically removed. There are also laparoscopic procedures that can be done manually or via robotic processes. There are also vaginal procedures, as well.
There are different types of hysterectomies, from complete to partial, and most of them are done using specific surgical procedures. For instance, there are “open” hysterectomies in which the patient is opened at the abdomen and the tissue and organs are surgically removed. There are also laparoscopic procedures that can be done manually or via robotic processes. There are also vaginal procedures, as well.
A 2014 article in the Wall Street Journal indicated that most women still opt for an open procedure, but that robotic and laparoscopic are a close tie. Interestingly enough, the, “American College of Obstetricians and Gynecologists… calls vaginal hysterectomies the best option.” (Levitz, 2014)
And while all of this debate would make for very interesting reading, there is one part of it that everyone must know about, and that is that some of the surgical options are now known to put women at risk for the development of aggressive cancer.
The Laparoscopic Connection
When a woman has a hysterectomy, it is going to involve the removal of a lot of tissue. The largest area to be removed is the uterus, and though a woman may be told that her fallopian tubes and ovaries will remain, the hysterectomy is always going to involve the removal of the uterus. Obviously, this can mean a lengthy recovery period and serious discomfort, but when this is done laparoscopically, it is minimally invasive and provides a much shorter period for recovery.
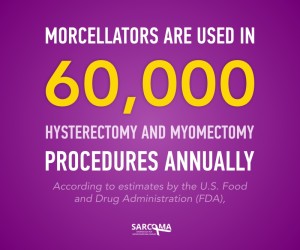
However, it also means that the tissue must be removed in a way that is radically different from the open or vaginal procedures. This is when a tool called a morcellator is put to use, and this is when women are put at such great risk for the development of cancer.
How? The morcellator enters the body in the same way that all laparoscopic tools do – through a tiny incision in the abdomen. At the tip of the tool is a device that effectively cuts, segments, and shreds the tissue to be removed, and then another device sucks it away. This sounds like a clean and effective treatment, but it is far from it. Instead, tiny cells and bits of tissue can be deposited throughout the abdominal cavity, and if a woman has undiagnosed Leiomyosarcoma (LMS) she can end up facing a very serious threat to her health and wellbeing.
This is because LMS is a rare form of soft tissue cancer that is quite treatable when caught early and when localized (in a single tumor). Because it is a sarcoma, though, it can spread to almost any area of the body. The use of the morcellator can release countless numbers of these deadly LMS cancer cells, and they can migrate throughout the abdomen and create a systemic case of LMS.
LMS & Hysterectomies
When it is systemic, LMS is often deadly because it does not respond well to chemotherapy or radiation. This means that a simple hysterectomy being done to give a woman comfort and freedom from the pain and hassles caused by fibroids can end up causing her to develop one of the most serious forms of cancer.
The FDA has recently warned against the use of morcellators during hysterectomy and myomectomy, and patients are advised to speak at great length with a doctor before allowing this tool to be used during their surgery.
Source
Levits, Jennifer. How Surgical Robots Spurred Morcellator Use in Hysterectomies. WSJ.com. 2014. http://www.wsj.com/articles/how-surgical-robots-spurred-morcellator-use-in-hysterectomies-1416600175
